5 Hidden Reasons for Inpatient Falls (And What Hospitals Often Miss)
Inpatient falls are one of the most common and serious safety events in hospitals. Between 700,000 and 1 million patients fall in U.S. hospitals every year and as many as 35 to 45 percent of those falls result in injuries such as fractures, head trauma, or longer hospital stays. Each fall with injury can add roughly $14,000 in costs and increase length of stay by nearly a week. Joint Commission International+1
Despite widespread prevention efforts, falls remain a persistent challenge because many contributing factors are subtle and easy to overlook. Here are five hidden reasons inpatient falls happen, and what hospitals are learning to address them.
1. Bed exit alarms fail silently because cables are broken or unplugged
Many fall prevention programs rely on bed exit alarms to alert staff when a patient attempts to leave the bed. These alarms can reduce fall risk when they work, and hospitals with strong sensor investments have reported up to 20–30% fewer falls compared with sites without these technologies. Becker’s Hospital Review
However, the technology only helps if it is connected and working correctly. A common yet underappreciated issue is that bed cables become damaged, disconnected, or are never plugged in, leaving alarms ineffective without staff knowing there’s a problem. When alarms fail silently, caregivers assume the system will alert them, even when it doesn’t.
This hidden failure point creates a false sense of security and can directly contribute to unassisted patient movements that lead to falls. Making alarm connectivity visible to staff and automated system checks part of routine monitoring helps close this gap.
2. Fall risk information does not follow the patient through transitions
Most hospitals conduct a fall risk assessment on admission, and these risks are clearly documented. But fall risk information often gets lost as patients move between units, shift changes occur, or care teams rotate.
Incomplete communication contributes to risks because caregivers may lack current visibility into a patient’s fall risk status. Hospitals facing this challenge find that relying on verbal handoffs or buried EHR notes is not enough, risk indicators need to be prominently visible across care transitions. Quality & Safety in Health Care
3. Alarm fatigue desensitizes staff and slows response
Alarms are everywhere in acute care environments, and many clinical teams report that alarm fatigue affects their ability to prioritize alerts. Although bed alarms can help reduce falls, they can also contribute to alert overload if not configured properly. Fall Prevention Foundation
When staff are exposed to frequent nuisance alerts, the result is slower responses even to the most critical ones. Tailoring alerts, routing them to the right devices, and reducing nonactionable triggers are crucial steps to ensure staff can respond swiftly to real fall risks.
4. Standard workflows assume perfect conditions
Preventing falls often depends on workflows built around ideal scenarios: staff are present, devices work as intended, and patients follow instructions. In reality, clinical environments are dynamic. Equipment gets damaged, batteries die, cables get disconnected, and patients can change status in the middle of a shift.
Because traditional fall prevention programs often assume things work right all the time, they miss the real operational failure points that lead to falls. Hospitals with better results design workflows that expect and manage imperfections by surfacing system status and errors early, rather than discovering issues after a fall occurs.
5. Technology is implemented without clear ownership
Fall prevention solutions – including alarms, sensors, and displays – often fall in the grey area between nursing, IT, facilities, and biomedical leadership. When no one group is clearly responsible for device maintenance and connectivity monitoring, small failures go unnoticed.
For example:
- Broken bed alarm cables sit unreplaced for weeks
- Sensor batteries remain dead
- Connectivity issues stay unresolved until after an incident
Clear ownership, routine checks, and accountability for fall prevention systems help ensure technology performs as expected and supports safe patient care.
The common thread in inpatient falls
Most falls are not caused by a single dramatic failure. Instead, they emerge from small gaps in visibility, communication, and system status that accumulate until a moment of risk becomes an incident.
From silent alarms with broken cables to fragmented fall risk communication, the pattern is consistent: when staff do not know the system is not working as intended, they operate as if it is.
Learn more about preventing falls with better bed connectivity
One of the biggest contributors to missed bed exit alarms is lack of visibility into bed connectivity status. Hospital teams that see and act on real-time device status can better trust their fall prevention systems.
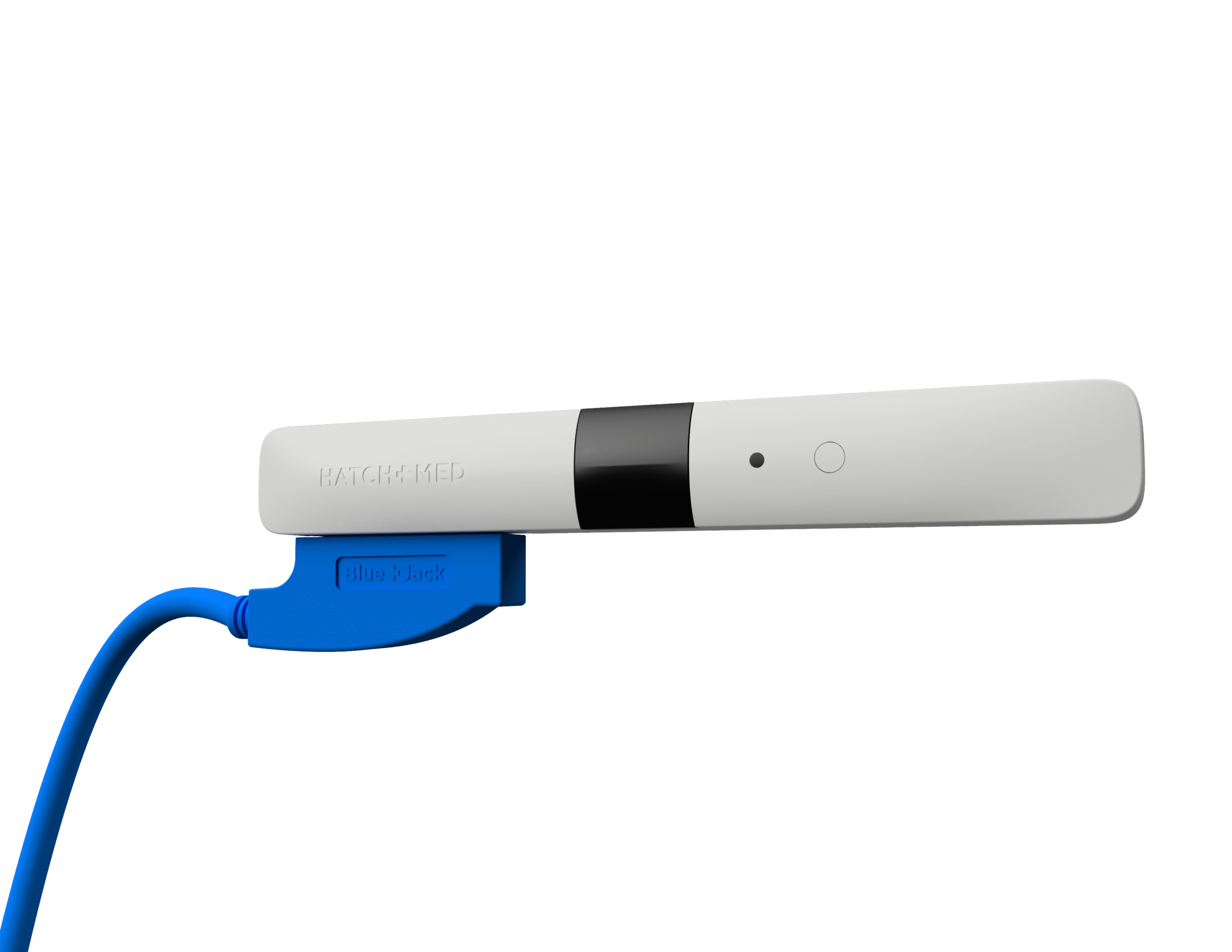
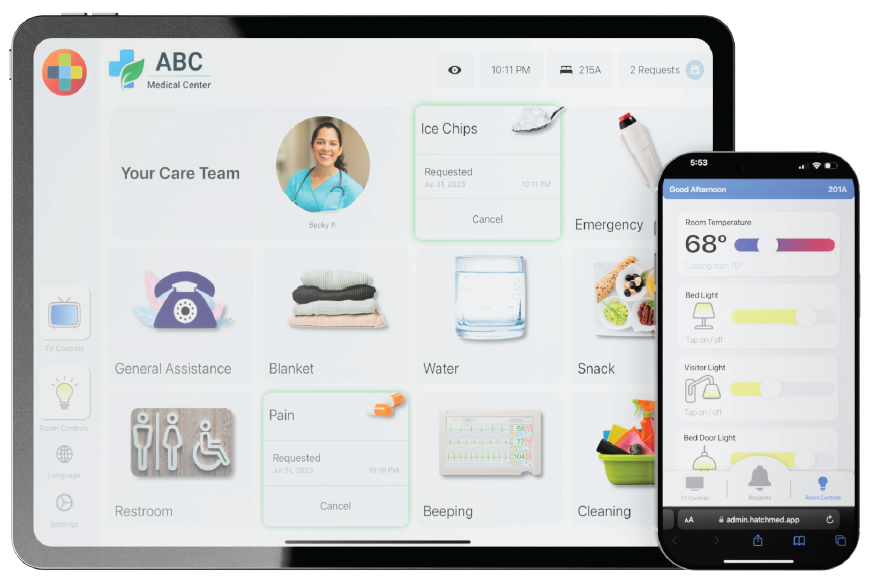
If you’re interested in how improved bed connectivity and real-time visibility can support fall prevention, check out HatchMed’s BlackJack solution, designed to make critical room-level data dependable and visible to care teams.
👉 Learn more about BlackJack and fall prevention